Eosinophils: Eosinophil Origin, Function and Related Conditions Including Eosinophilia
Frontline immune cell plays an important part in allergy and battling parasitic infections
Complete the form below to unlock access to ALL audio articles.
Immune cells are a group of cells dedicated to defending our bodies from all things “non-self”. Within the group there are members that perform different tasks and that specialize in different functions, working together to the overcome multiple threats we face on a daily basis.
In this article, we consider what eosinophils are, how they are generated, their function in the body and medical conditions related to them, including eosinophilia.
What is an eosinophil?
Eosinophils, like basophils and neutrophils belong to the granulocyte group of immune cells. They were first described by Paul Ehrlich in 18791 and are part of the frontline, innate immune system, playing an important role in the prevention of parasitic infections, asthma and allergic reactions.
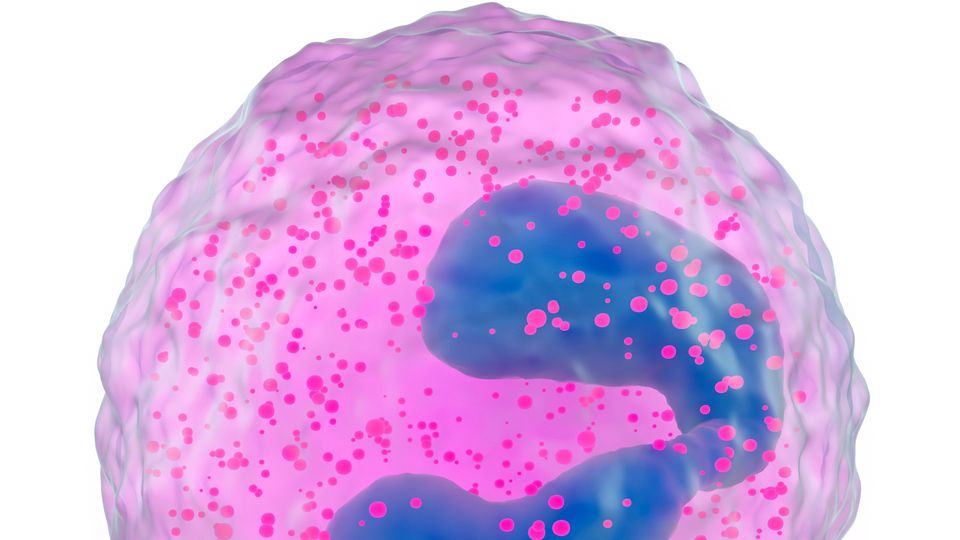
About 1–5% of circulating leucocytes found within the body are eosinophils. They have a cytoplasm containing coarse, round granules of uniform size that stain readily with eosin and other acid dyes. The granules contain amongst other enzymes, arginine- and zinc-rich basic protein, peroxidase, acid phosphatase, phospholipase B and D, histaminase, ribonucleases, β-glucuronidase, cathepsin and collagenase. The cells are 10–17 microns in diameter and have predominantly bi-lobed, equal sized nuclei linked by chromatin.2
Eosinophils are generated in the bone marrow and start life as multipotent hematopoietic stem cells with the ability to differentiate into multiple different cell types. As with basophils, the stem cells must differentiate into a myeloid progenitor cell or myoblast with the shared properties of both types of cell, and then further on into the specific eosinophil lineage (Figure 1).3 Eosinophil generation is determined by an array transcription factors and signaling molecules including GATA-1, interleukin 3 (IL-3) and interleukin 5 (IL-5).4 Eosinophil progenitor cells mature into fully functional eosinophils within the bone marrow and are then released into the bloodstream, after which they do not normally multiply. Once in the bloodstream they have a relatively short lifespan of between 8 and 18 hours. After circulating in the blood, they migrate to the tissues, in response to chemokines, where they typically have a lifespan of between 2–5 days, which may be increased by cytokine release.5
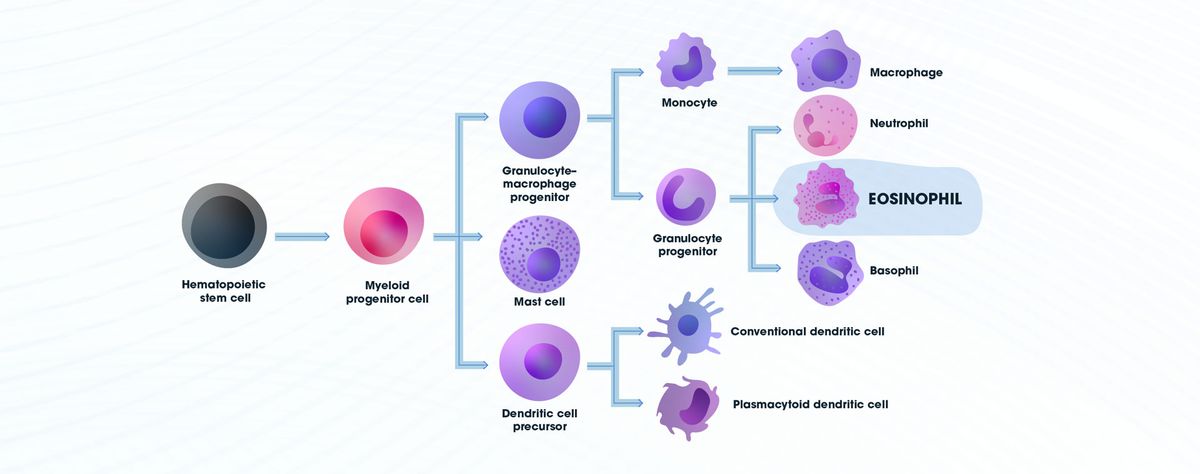
Figure 1: Diagram showing the differentiation pathway for the development of eosinophils. Credit: Technology Networks.
Eosinophil function
Eosinophils exert their effector functions in a variety of ways, especially in response to parasitic infection, inflammatory responses and allergic reactions.6 Eosinophil granules contain a wide variety of enzymes and other chemicals that are released in the process of degranulation (Figure 2). They are particularly renowned for their response to parasitic infections, where, upon contact, they are stimulated to release their toxic contents, including eosinophil peroxidase (EPX), major basic protein (MBP-1), eosinophil cationic protein (ECP) and eosinophil-derived neurotoxin (EDN), which can help to eliminate the parasite. A variety of lipid mediators and numerous cytokines and chemokines that are capable of stimulating other immune cells, including T cells, B cells and dendritic cells, can also be released by eosinophils, influencing the overall immune and inflammatory responses.7
Additionally, eosinophils play a role in a number of allergic reactions, interacting with IgE and allergens, which stimulates degranulation, and the proteins released contributing to the inflammatory responses at the site of exposure. This process can become chronic if the exposure continues, leading to tissue damage and organ failure or rejection caused by the cytotoxic enzymes released. They are also capable of interacting with mast cells to form an “allergic effector unit”, associated with allergic reactions and some tumors.8
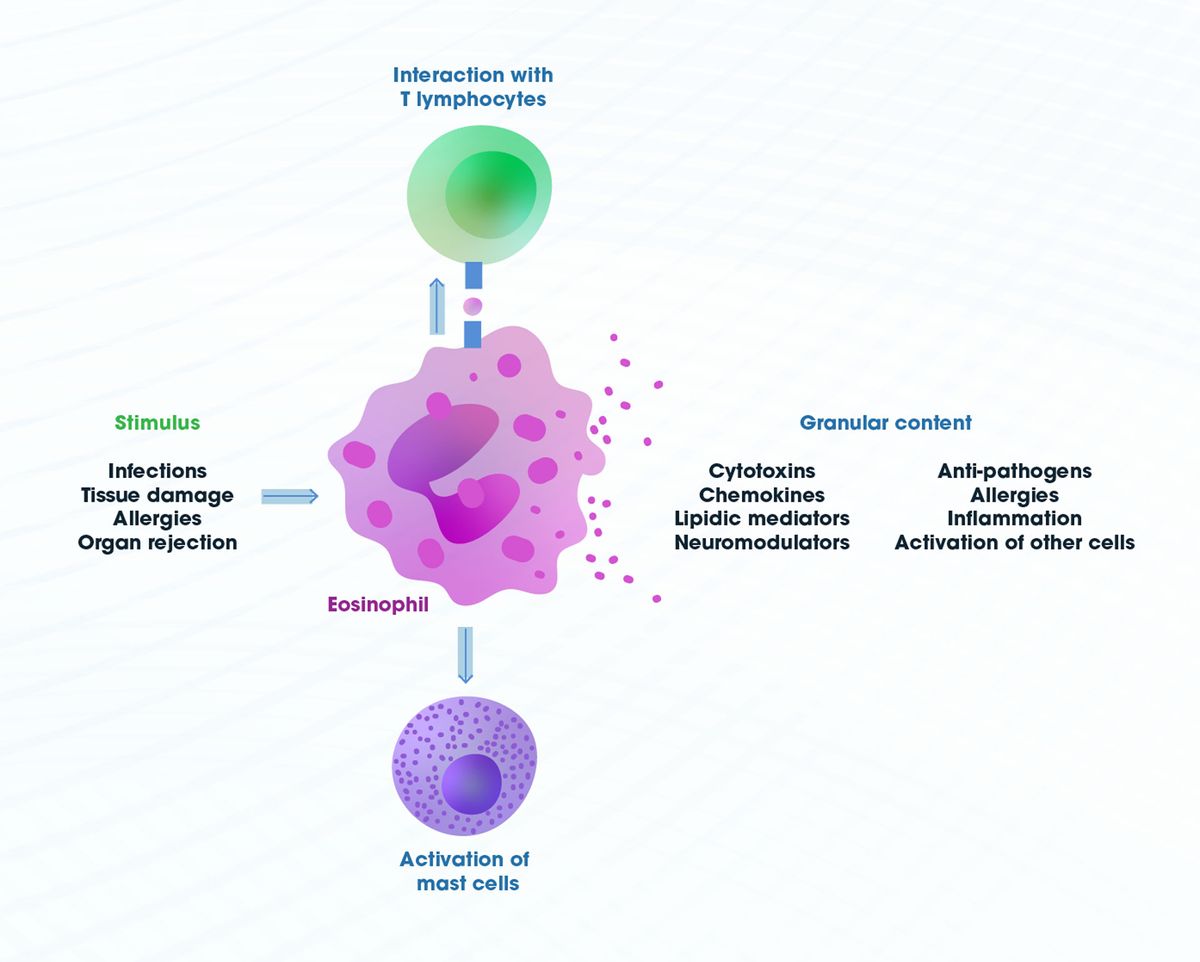
Figure 2: Eosinophil stimuli, interactions and mediators. Credit: Technology Networks.
Bacterial phagocytosis has been observed by eosinophils, however, it is less efficient than that observed in neutrophils and is associated with degranulation and the release of lysosomal enzymes.9 In addition to the inflammatory processes associated with eosinophils, they have also been shown to play a role in non-inflammatory activities and in the generation and maintenance of adaptive immune responses and, be needed for tissue integrity and tissue remodeling.10
What is eosinophilia?
Eosinophilia is a term describing an abnormal increase in the number of eosinophils. They are typically present in low numbers in the blood and when their levels become significantly elevated, it can be a sign of an underlying medical condition. Eosopenia on the other hand is a lower-than-normal level of eosinophils in the blood and is often transient and non-specific as it observed in a variety of clinical conditions.
Eosinophil-related conditions
A bodily environment that produces the stimulatory molecules and circumstances to promote eosinophil proliferation and activation can lead to eosinophilia, while other circumstances, such as stimuli resulting in degranulation, can reduce circulating eosinophil numbers. Let’s consider some examples.
Eosinophilia11
- Eosinophils are involved in the body's response to parasitic infections and thus infestation with parasitic worms can lead to eosinophilia.
- Some medications can cause eosinophilia as a side effect. This may occur in response to antibiotics, anticonvulsants and non-steroidal anti-inflammatory drugs (NSAIDs), among others.
- Eosinophilia is commonly associated with allergic diseases, such as asthma, hay fever and allergic skin conditions.
- Certain autoimmune disorders, such as eosinophilic granulomatosis with polyangiitis (formerly known as Churg–Strauss syndrome), can lead to elevated eosinophil levels.
- One rare condition that can lead to eosinophilia is hyper eosinophilic syndrome (HES); it is characterized by persistently elevated eosinophil counts and is generally idiopathic. The condition can lead to organ damage due to tissue infiltration by eosinophils.
- Acute and chronic eosinophilic leukemia are eosinophil-derived malignancies and are associated with eosinophilia.
- Autosomal-dominant hyper-IgE syndrome (Job syndrome), Wiskott–Aldrich syndrome and Omenn syndrome are immunodeficiency-related conditions that all result in eosinophilia.
- Eosinophilia has also been associated with the rejection of transplanted organs.
Eosinopenia12
- Eosinopenia may occur during acute bacterial infection periods. The body may release cortisol that can reduce the number of circulating eosinophils by suppressing the release of proinflammatory cytokines like IL-5. This can also occur during periods of acute stress where release of cortisol suppresses the release of eosinophils.
- Severe sepsis and systemic inflammatory response syndrome (SIRS), which are associated with widespread inflammation, can lead to a decrease in eosinophil levels as they degranulate to try and combat the infection.
- The use of corticosteroid medications, commonly prescribed for inflammatory conditions or autoimmune diseases, can lead to a decrease in eosinophil levels by suppressing immune cell generation.
- Cushing's syndrome, a disorder characterized by prolonged exposure to high levels of the hormone cortisol, can be associated with eosinopenia, again by inhibiting the production of pro-inflammatory cytokines.
- A sudden and severe deficiency of adrenal hormones, such as in acute adrenal insufficiency or Addisonian crisis, can result in eosinopenia by stimulating the body to move eosinophils from the circulation and into tissues.
Eosinophils are generally considered to be vital to the body’s defense against certain pathogens and have been shown to have multiple regulatory functions within our bodies. However, in certain circumstances when their numbers become altered and their function becomes unregulated they can contribute to organ failure and tissue damage.
1. Ehrlich P. Über die specifischen granulationen des blutes. Arch Anat Physiol (Leipzig). 1879. 571–579.
2. Wickramasinghe SN and Erber WN. Normal blood cells. In: Porwit A, McCullough and Erber WN eds. Blood and Bone Marrow Pathology (Second Edition). Churchill Livingston. 2011:3-18. doi:10.1016/C2009-0-52942-X
3. Boyce JA, Friend D, Matsumoto R, Austen KF and Owen WF. Differentiation in vitro of hybrid eosinophil/basophil granulocytes: Autocrine function of an eosinophil developmental intermediate. J. Exp. Med. 1995;182:49. doi:10.1084/jem.182.1.9
4. Uhm TG, Kim BS and Chung IY. Eosinophil development, regulation of eosinophil-specific genes, and role of eosinophils in the pathogenesis of asthma. Allergy Asthma Immunol Res. 2012; 4(2):68–79. doi:10.4168/aair.2012.4.2.68
5. Park YM and Bochner BS. Eosinophil survival and apoptosis in health and disease. Allergy Asthma Immunol Res. 2010;2(2):87-101. doi:10.4168/aair.2010.2.2.87
6. Fettrelet T, GigonL, Karaulov A, Yousefi S and Simon H-U. The enigma of eosinophil degranulation. Int J Mol Sci. 2021; 22(13):7091. doi:10.3390/ijms22137091
7. Wen T and Rothenberg ME. The regulatory function of eosinophils. Microbiol Spectr. 2016;4(5). doi:10.1128/microbiolspec.MCHD-0020-2015
8. Galdiero MR, Varricchi G, Seaf M et al. Bidirectional mast cell–eosinophil interactions in inflammatory disorders and cancer. Front. Med. 2017;4(103). doi:10.3389/fmed.2017.00103
9. Shamri R, Xenakis JJ and Spencer LA. Eosinophils in innate immunity: An evolving story. Cell Tissue Res. 2011; 343(1): 57–83. doi:10.1007/s00441-010-1049-6
10. Lombardi C, Berti A and Cottini M. The emerging roles of eosinophils: Implications for the targeted treatment of eosinophilic-associated inflammatory conditions. Current Res Immunol. 2022;3:42-53. doi:10.1016/j.crimmu.2022.03.002
11. Kovalszki, A and Weller PF. Eosinophilia. Prim Care. 2016;43(4): 607–617. doi:10.1016/j.pop.2016.07.010
12. Zini G. Abnormalities in leukocyte morphology and number. In: Porwitt A, McCullough J and Erber WN eds. Blood and Bone Marrow Pathology (Second Edition). Churchill Livingstone. 2011:247-261. doi:10.1016/B978-0-7020-3147-2.00016-X